Stroke 101: Know the Signs. Act Fast. Save Lives
Written by Dr. Illingworth | July 30th 2025
What Is a Stroke?
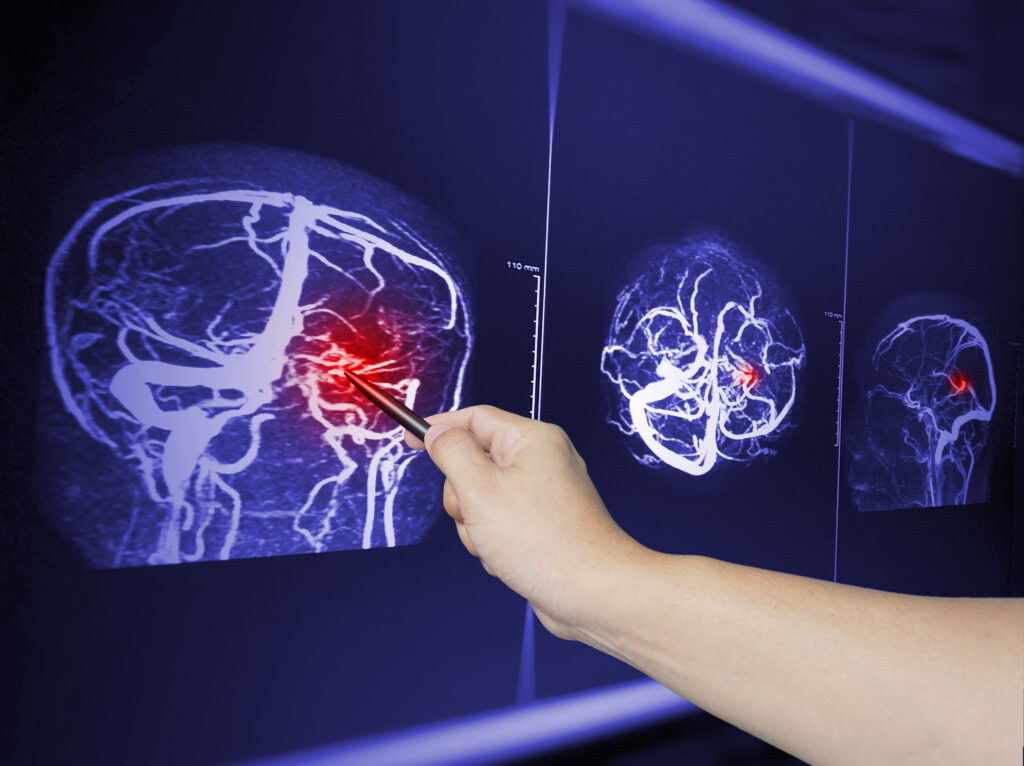
A stroke occurs when there is an interruption or reduction in blood flow to a portion of the brain. This lack of blood flow prevents brain tissue from receiving the oxygen it needs. As a result, brain cells can begin to die within minutes. A stroke is considered a medical emergency, and prompt action is critical to minimizing brain damage and potentially saving lives.
Ischemic stroke
A blockage of a blood vessel in the brain can lead to an ischemic stroke, which is the most common type of stroke. This blockage often occurs due to blood clots forming in arteries that have been damaged by plaque, a condition known as atherosclerosis. In some cases, clots may travel from other parts of the body, a process called embolism. Other factors, such as fat embolism, infections, and inflammation, can also contribute to blockages.
Ischemic strokes are often treated with clot-busting medication (tPA or tNK) and/or mechanical thrombectomy if caught early enough. Following these initial interventions, patients typically receive antiplatelet therapy. It’s essential to recognize that the exact treatment can differ based on the specific cause of the blockage in each case.
Hemorrhagic Stroke
A hemorrhagic stroke occurs when a blood vessel in the brain bursts, leading to bleeding into or around the brain. This type of stroke is often caused by factors such as high blood pressure, aneurysms, or head trauma. Immediate medical care is required to control the bleeding and reduce pressure on the brain, which may involve surgical intervention. Prompt treatment is crucial for minimizing damage and improving outcomes.
A Transient Ischemic Attack (TIA)
Occurs due to a temporary blockage of blood flow to the brain. The symptoms
typically last for a few minutes to a few hours. They should resolve within 24 hours, without any neuroimaging findings. It’s essential to pay attention to TIAs, as they serve as a significant warning sign that a full stroke may be imminent. Immediate evaluation and medical attention are crucial to address any underlying issues and to reduce the risk of a more severe stroke occurring in the future.
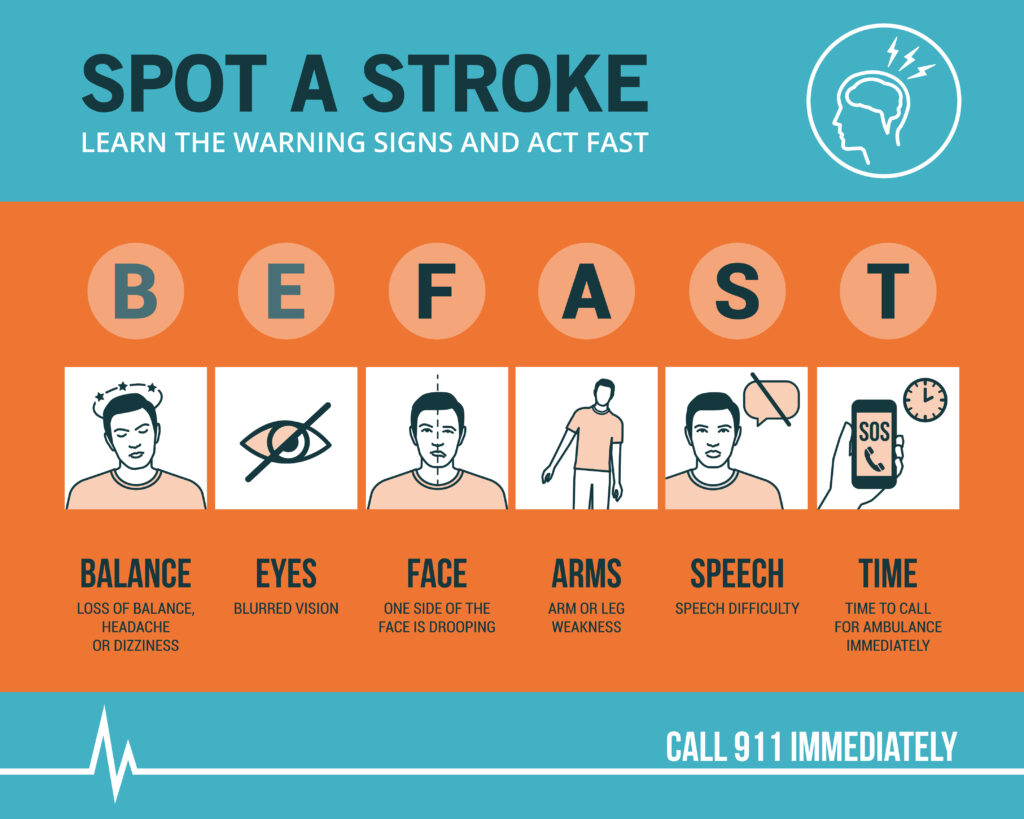
When a stroke occurs, recognizing the symptoms quickly can make a significant difference. The acronym F.A.S.T. helps to remember the warning signs:
Face drooping: Face drooping is a key warning sign of a stroke. If you notice that one side of the face appears to droop, or if the person seems to have numbness in that area
Arm weakness: Arm weakness is another critical symptom of a stroke. To assess this, ask the person to raise both arms. If one arm feels weak or numb and drifts downward while the other remains steady, this could indicate a potential neurological deficit.
Speech difficulty: If the person’s speech is slurred, garbled, or if they are unable to speak at all, it may suggest that they are experiencing a stroke.
Time to call 911: If you notice any of these signs, it’s crucial to act quickly. Call 911 immediately for emergency services. Time is vital in these situations, as seeking prompt medical attention can significantly affect outcomes and recovery. Don’t hesitate; every minute counts!
In addition to the main warning signs of a stroke, there are other symptoms to be aware of:
-
- Sudden confusion or trouble understanding others: A person may seem
disoriented or unable to comprehend what’s being said. - Sudden trouble seeing: Vision changes can happen in one or both eyes,
leading to blurred, double, or lost vision. - Sudden difficulty walking: This can include dizziness, loss of balance, or
problems with coordination. - Sudden severe headache: A headache that strikes suddenly and has no known cause could indicate a hemorrhagic stroke.
- Sudden confusion or trouble understanding others: A person may seem
Stroke can affect anyone, but certain factors can increase your risk of having a stroke. These factors can be categorized into modifiable and non-modifiable risk factors:
Modifiable risk factors:
- High blood pressure: Often the leading cause of strokes.
- Diabetes: Increases the risk due to potential damage to blood vessels.
- High cholesterol: Can lead to plaque buildup in arteries.
- Smoking: Contributes to vascular problems and increases stroke risk.
- Obesity: Excess weight can contribute to other risk factors.
- Sedentary lifestyle: Lack of physical activity can lead to other health issues.
- Excessive alcohol use: Can increase blood pressure and lead to other health
problems. - Sleep apnea: This condition can contribute to high blood pressure and other
issues. - Atrial fibrillation: An irregular heartbeat increases stroke risk due to possible
blood clots.
Non-modifiable risk factors:
- Age: The risk of having a stroke increases as you get older.
- Family history: A family history of stroke can increase your risk.
- Race/ethnicity: Certain populations may have a higher risk.
- Gender: Women may tend to have worse outcomes when experiencing a
stroke.
Understanding these risk factors can help you take preventive measures and seek timely medical advice.
Why Acting Quickly Matters
Acting quickly during a stroke is crucial because every minute counts. Nearly 2 million brain cells can die every minute due to the lack of blood flow. The sooner treatment is initiated, the greater the chances for recovery. For example, treatments like tPA can only be given within the first 3 to 4.5 hours after symptoms start.
Recognizing the signs of a stroke and calling 911 immediately is essential. You should not attempt to drive to the hospital. Emergency medical teams are trained to implement stroke protocols while en route, which helps minimize the time until treatment can begin. Prompt action can significantly improve outcomes and recovery chances.
